Conditions We Treat
Diabetic Ulcers
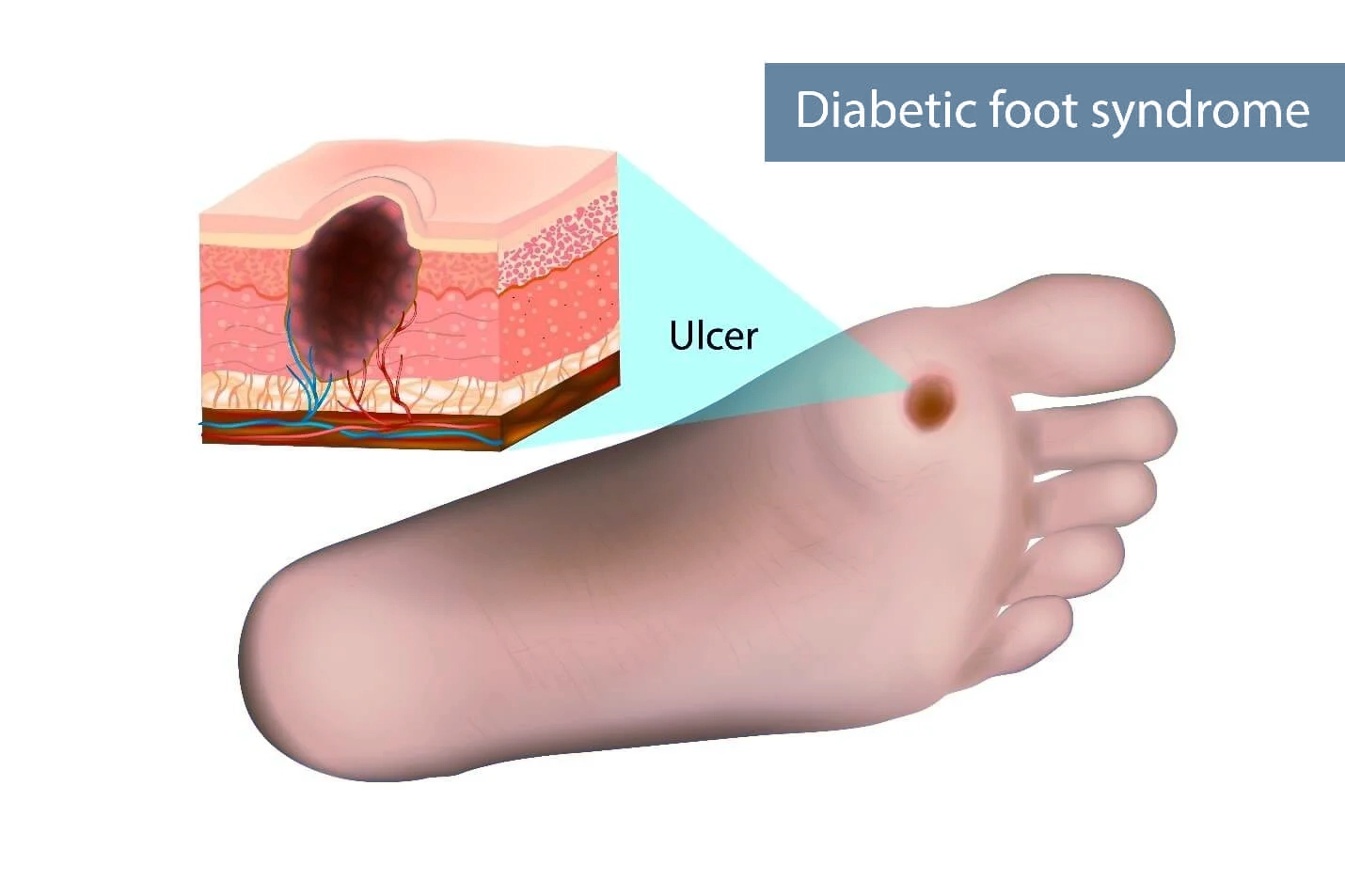
What Are Diabetic Ulcers?
How Do I Know if I Have a Diabetic Ulcer?
How Can I Perform Diabetic Wound Care at Home?
Before beginning any at-home diabetic foot ulcer treatment, you must visit your physician. Your physician will evaluate your overall health, determine the underlying cause of the ulcer, evaluate its severity, and check for infection. They may also clean and debride the wound, dress it for you, and prescribe antibiotics. If the ulcer is not serious enough to require surgery or a hospital stay, you will be given wound care instructions for home care. The best ways to treat diabetic ulcers at home are:
- Clean the ulcer at least once daily with soap and water. Your physician may recommend another type of cleanser. Do not soak your wound in a bath, pool, or hot tub, or use Epsom salts or hydrogen peroxide.
- Keep your ulcer loosely covered with an antimicrobial dressing. Keeping a wound uncovered can increase your risk of infection and slow the healing process.
- Apply antibiotic gel or cream or take antibiotic pills as your physician recommends.
- Manage your diabetes, maintain a healthy diet, and keep your blood sugar under control.
What Are Common Diabetic Foot Complications?
Being aware of the complications of diabetic ulcers can ensure you’re able to get the help you need before an issue gets worse or more dangerous. The most common complications of diabetic ulcers are:
- Diabetic Foot Infections – The most common complication of a diabetic ulcer is infection. The ulcer can get infected if it goes unnoticed or untreated for too long if it is not cared for properly, or if bacteria gets in the wound. You may have an infection if you have swelling around the wound site, yellow liquid oozing from the wound, discharge, a foul odor from the wound, fever or chills, and hot, tight, red skin around the wound.
- Abscesses – If an infection isn’t treated, you may develop an abscess. An abscess is an accumulation of pus under the skin. It will look swollen, bulbous, larger than usual, and may have a small hole where it oozes pus.
- Sepsis – Sepsis can occur if an infection gets deep enough to enter your bloodstream and can be life-threatening. Symptoms of sepsis include trouble breathing, blue or blotchy skin, sweating, lightheadedness, shivering, disorientation or confusion, and a fast heart rate.
- Deformity – If you have long-term uncontrolled diabetes or a long-term diabetic foot infection, the muscles and bones in your foot can weaken. This can cause deformity and possibly even fractures or dislocations of the foot.
- Gangrene – Gangrene or tissue necrosis can occur when an infection causes a loss of blood flow to the foot. The initial signs of gangrene are loss of sensation in the affected area, blisters, swelling, severe pain followed by numbness, cool or cold skin, thin and shiny skin, a foul-smelling discharge, and black tissue.
- Diabetic Foot Surgery or Amputation – If you have a severe enough infection or gangrene, you may need surgery to remove infected or necrotic tissue. If you have neuropathy, peripheral arterial disease, or gangrene, you may need to have your foot amputated.
What Are Some Diabetic Ulcer Prevention Tips?
If you are at risk of diabetic ulcers, you can take measures to reduce your risk. Your physician will give you instructions for managing your diabetes and lowering your risk of ulcers. You should:
- Keep your blood sugar under control.
- Get daily exercise.
- Maintain a healthy diet.
- Check your skin every day for cuts, wounds, sores, blisters, calluses, white spots, redness, and cracks. You should also feel the area for warmth or to see if it is colder than usual.
- Quit smoking.
- Manage your blood pressure and cholesterol.
- Care for your toenails.
- Avoid walking barefoot or wearing uncomfortable or poorly fitting shoes.
Call Today for Mobile Wound Care for Diabetic Ulcers
Common Conditions We Treat
Featured Treatments We Provide












